Helping Children Transition Between Seasons: Why Spring Can Be Hard for Some Kids
For many families, spring brings warmer weather, longer days, and a sense of renewal. But for some children — especially those with autism — seasonal changes can feel overwhelming rather than exciting. Shifts in routine, sensory input, and daily structure can create challenges that aren’t always obvious at first.
Understanding why these transitions are hard — and how ABA therapy can help — allows families to move through seasonal changes with more confidence and less stress.
Why Seasonal Transitions Can Be Difficult for Autistic Children
Children on the autism spectrum often thrive on predictability and routine. When seasons change, many subtle and not-so-subtle differences occur all at once.
Some of the most common challenges include:
🌿 Changes in Routine
Spring often means different school schedules, outdoor activities, holidays, and shifting expectations. Even positive changes can feel destabilizing when routines are disrupted.
☀️ Sensory Shifts
Spring brings new sensory input: brighter sunlight, warmer temperatures, stronger smells, pollen, buzzing insects, and different clothing textures. For sensory-sensitive children, these changes can feel intense or uncomfortable.
⏰ Changes in Daylight
Longer daylight hours can affect sleep patterns, energy levels, and mood regulation. Children who already struggle with sleep or transitions may find it harder to settle into new rhythms.
🧠 Increased Cognitive Demands
With spring comes more social interaction, outdoor play, and transitions between environments — all of which require flexibility, communication, and emotional regulation.
When several of these factors happen at once, it’s common for families to notice more meltdowns, withdrawal, anxiety, or regression in certain skills.
How ABA Therapy Supports Seasonal Transitions
ABA therapy focuses on teaching children the skills they need to navigate real-life changes — including seasonal ones — with greater independence and confidence.
Here’s how ABA helps during transitions like spring:
✔️ Strengthening Emotional Regulation
ABA therapists help children identify feelings, build coping strategies, and practice calming techniques so they can manage frustration or sensory overwhelm more effectively.
✔️ Building Flexibility
Through structured practice and positive reinforcement, children learn how to tolerate changes, adapt to new routines, and respond to unexpected situations.
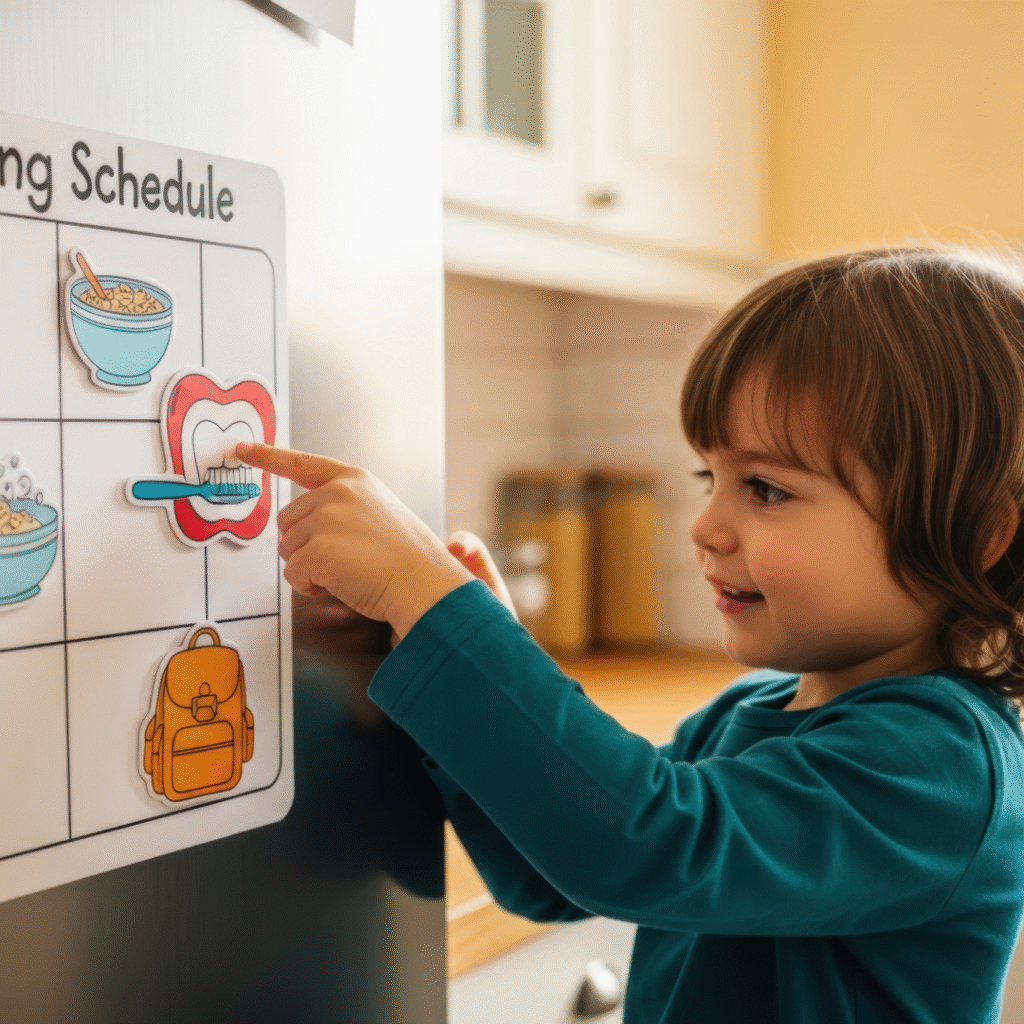
✔️ Using Visual Supports
Visual schedules, First/Then boards, and social stories help children understand what is changing, what stays the same, and what to expect next — reducing anxiety and uncertainty.
✔️ Supporting Communication
ABA therapy teaches children how to express discomfort, ask for breaks, or request support instead of communicating distress through behavior alone.
✔️ Practicing in Real Environments
Therapists often work in natural settings — homes, schools, and communities — allowing children to practice coping with seasonal changes where they actually happen.
Practical Tips for Families During Seasonal Changes
Parents and caregivers play a huge role in helping children feel safe and supported through transitions. Here are some ABA-informed strategies you can use at home:
🌸 Keep Routines as Predictable as Possible
Even when schedules change, try to maintain consistency in key parts of the day: meals, bedtime, morning routines, and therapy times.
📆 Use Visuals to Prepare for Change
Show upcoming schedule changes visually. A simple calendar or picture schedule can reduce anxiety by making change more concrete and understandable.
🧢 Prepare for Sensory Differences
Spring means different clothes, brighter light, and outdoor textures. Allow your child to adjust gradually, and offer sensory tools like hats, sunglasses, or fidget items as needed.
😴 Support Healthy Sleep
Longer daylight can disrupt sleep. Use blackout curtains, consistent bedtime routines, and calming activities to help your child wind down.
🗣 Talk Through Changes Ahead of Time
Use simple, clear language to explain what will be different and what will stay the same. Repetition helps children feel secure.
🌱 Celebrate Small Wins
Adjusting to seasonal change is a big task! Acknowledge progress — even small moments of flexibility or calm — to build confidence.
When to Seek Extra Support
If your child experiences increased distress, regression in skills, or significant difficulty adjusting during seasonal changes, it may be helpful to seek professional support. ABA therapy can offer personalized strategies that address your child’s specific needs and challenges.
Early support can prevent small difficulties from becoming larger barriers to learning, comfort, and independence.
Seasonal transitions like spring bring growth and possibility — but for some children, they also bring real challenges. With understanding, preparation, and the right support, these changes can become opportunities for learning, resilience, and skill-building.
ABA therapy doesn’t just address behaviors — it helps children build the emotional and practical tools they need to thrive through change.


 1. Nature Walk & “I Spy” Scavenger Hunt
1. Nature Walk & “I Spy” Scavenger Hunt Choose a quiet park or trail
Choose a quiet park or trail 2. Leaf Sorting & Sensory Exploration
2. Leaf Sorting & Sensory Exploration Gently rub leaves between fingers to feel the texture
Gently rub leaves between fingers to feel the texture Blow leaves off a table to support breath control
Blow leaves off a table to support breath control 3. Pumpkin Painting (Not Carving)
3. Pumpkin Painting (Not Carving) Brush painting for low-mess sensory input
Brush painting for low-mess sensory input Stickers, googly eyes, or sponge painting
Stickers, googly eyes, or sponge painting 4. Fall-Themed Sensory Bins
4. Fall-Themed Sensory Bins Hide letters or picture cards inside
Hide letters or picture cards inside Practice turn-taking and requesting items
Practice turn-taking and requesting items Label objects to build vocabulary
Label objects to build vocabulary 5. Apple Taste Test & Cooking Activity
5. Apple Taste Test & Cooking Activity Sliced apples (different types)
Sliced apples (different types) Warm apple crisp or baked cinnamon apples
Warm apple crisp or baked cinnamon apples 6. Cozy Corner with Autumn Sensory Items
6. Cozy Corner with Autumn Sensory Items Soft blanket
Soft blanket Fall-scented diffuser (if tolerated)
Fall-scented diffuser (if tolerated) Autumn-themed books
Autumn-themed books 7. Costume Dress-Up Practice (Without the Halloween Stress)
7. Costume Dress-Up Practice (Without the Halloween Stress)
 What Is After-School Restraint Collapse?
What Is After-School Restraint Collapse? Why Meltdowns Happen After School
Why Meltdowns Happen After School How ABA Therapy Can Help
How ABA Therapy Can Help Practical Tips for Parents Right Now
Practical Tips for Parents Right Now Final Thoughts
Final Thoughts
